Activities
Advance Care Planning Community Outreach
Upcoming Events
Free Workshop: Advance Directive
August 2025 (Date and Time TBD)
Held at
Hopewell House.
Background
A humane and effective health care system cares for both its patients and for the people working in the system itself. But when it comes to end-of-life care, our system is failing both groups. Many patients arrive at end-of-life incapacitated and unable to articulate their specific wishes regarding care and comfort measures, leaving those decisions to unprepared loved ones who often opt for extreme measures out of a sense of duty and caution. As a result, health care workers are often tasked with prolonging end-of-life patients' decline and suffering, leaving those health care workers demoralized and exhausted, both mentally and physically. It's a vicious and self-defeating cycle. Fortunately, there is a ready solution: Advance Care Planning (ACP) - a formalized process for discussing and preparing for an individual's future medical care.
Why Community Outreach?
In the quarter century that I have been practicing as a physician, I've seen few, if any, improvements in the practice of "Preparing for Future Medical Care." Thus, I decided to reach out to the community in-person to share the importance of ACP. Even though these efforts sometimes feel like a drop in the ocean, what continues to motivate me is seeing other medical team members, like myself, increasingly experience moral distress around end-of-life care, thus threatening the loss of our medical system's vital workforce.
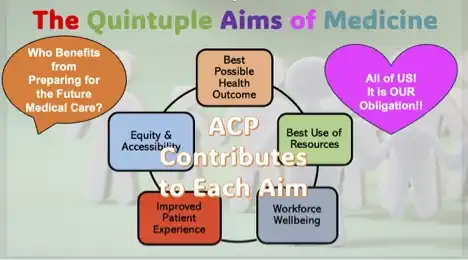
ACP Contributes to Each Quintuple Aims of Medicine
I am inspired by the "Quintuple Aims of Medicine" which represents the ideal state of our healthcare system. Advance Care Planning (ACP) practice directly contributes to each of these aims.
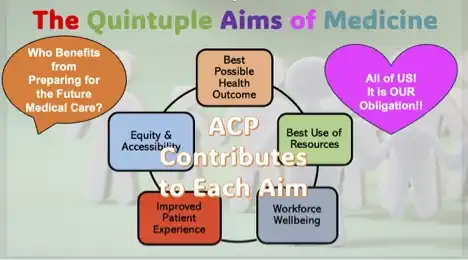
Improving Patient Experience Will Improve Workforce Wellbeing
Unless we commit ourselves to improving our medical system, it will not happen. Each of us can contribute to improving the system by preparing for our own future medical care. By doing so, we can improve our individual/patient “experience” in medical care, and in turn, improve overall “workforce wellbeing.” I see these as very important components to improving the system.
Your Line in the Sand
Preparing for future medical care ultimately means thinking about your own view of ''Quality of Life (QoL).'' Most of us have our own standards for QoL, based on specific levels of disabilities in which we might find ourselves. No one can truly predict what will be unacceptable to another person - it is utterly individual and entirely subjective. You are the only person who can tell anyone what your priorities are, thus your medical team will want to hear your “voice” on the subject, even if you cannot speak for yourself.
Appoint your Surrogate Decision Maker(s)
That is why you need to appoint a health care advocates, in advance, and ideally both by person and by document, especially if you choose not to. When your medical team knows where you have drawn your ''lines in the sand,'' it will help them to reach your individual ''Best Possible Health Outcome'' and ''Best Use of Resources.'' We always have limited resources, but fortunately we can also always improve our use of those resources to improve ''Equity & Accessibility.''
Join the Community ACP Movement
Since 2023 my colleagues and I have worked together to spread the word about ACP. As of November 2024, we have met with over 800 community members and given over two dozen public presentations and workshops to get ordinary people exited about ACP.
We are happy to work with you to inform and assist your community in preparing for future medical care!
To begin the process, please contact me at
me@erikoonishi.com.
You can also download my informative presentations on ACP (in PDF format) here: